|
Getting your Trinity Audio player ready...
|
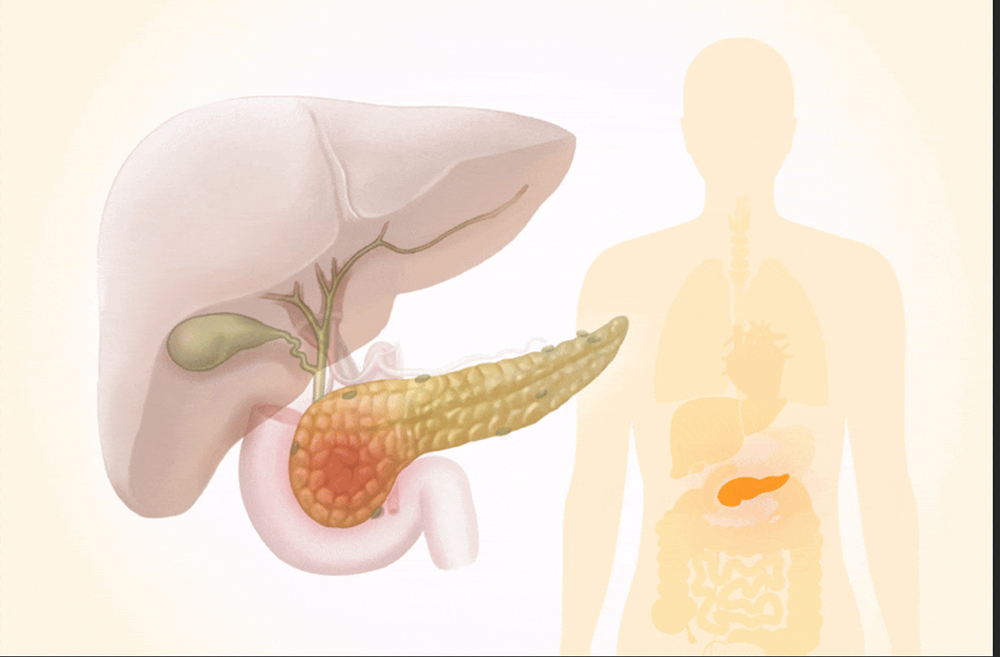
Though only six inches long, the pancreas plays a vital role in digestion and blood sugar regulation.
By: Mercura Wang
Pancreatic cancer is among the deadliest forms of cancer. Although it accounts for only about 3 percent of all cancer cases, it is responsible for a disproportionately high number of cancer-related deaths.
One reason for pancreatic cancer’s high mortality rate is that it’s often diagnosed at an advanced stage. By the time it’s detected, treatment options are limited.
Understanding the symptoms and the risk factors is a critical first step toward prevention.
What Are the Symptoms and Stages of Pancreatic Cancer?
Pancreatic cancer is notoriously difficult to detect early because symptoms are easily overlooked. By the time most cases are diagnosed, about 90 percent have already spread to nearby tissues, lymph nodes, or distant organs such as the liver or lungs.
Some patients may experience only one symptom, while others may have several. Symptoms can also vary greatly from person to person.
Belly or Back Pain: Pain is more common in cancers that develop in the body or tail of the pancreas. The pain is often described as dull or gnawing, may come and go at first, and typically starts in the upper abdomen, sometimes spreading to the sides or back. It can worsen after eating or when lying down.
Jaundice: This symptom may occur when tumors form in the head of the pancreas, near the bile duct. A blocked bile duct causes a buildup of bilirubin—a yellowish substance—in the body. Jaundice can also lead to dark urine, pale or greasy stools, and itchy skin.
Unexplained Weight Loss: More common in cancers that start in the head of the pancreas, often accompanied by loss of appetite.
Stool Changes: A blocked pancreatic duct may lead to fatty, pale, foul-smelling stools that are difficult to flush, indicating poor nutrient absorption and possible weight loss. Other bowel changes may include diarrhea or constipation.
Indigestion: This can lead to symptoms such as heartburn, bloating, and nausea.
Certain conditions might indicate signs of pancreatic cancer:
Blood Clots: Pancreatic cancer promotes blood clots by releasing clot-triggering proteins such as tissue factor and thrombin, and by altering blood composition to increase clotting factors. A blood clot in a large vein—known as deep vein thrombosis—may cause leg pain, swelling, redness, and warmth. If part of the clot breaks off and travels to the lungs, it can cause a pulmonary embolism—a sudden blockage in one of the arteries in the lungs—leading to chest pain or difficulty breathing.
Diabetes: Pancreatic cancer can damage the insulin-producing cells in the pancreas, leading to high blood sugar and diabetes. This may cause increased thirst, hunger, and frequent urination.
Gallbladder Enlargement: If the bile duct becomes blocked by cancer, bile can accumulate in the gallbladder, causing it to enlarge.
Advanced Symptoms
When pancreatic cancer spreads to other parts of the body, it causes location-specific symptoms:
If Spread to the Liver or Abdomen: Pain on the right side of the abdomen and ascites—swelling from fluid buildup. Pancreatic cancer may also lead to an enlarged liver, even before the cancer has spread to that area.
If Spread to the Lungs: Persistent cough, shortness of breath, recurring chest infections, coughing up blood, and pleural effusion—fluid between the lung and chest wall.
If Spread to the Bones: Weak or easily broken bones; high blood calcium levels, which can cause dehydration, confusion, nausea, abdominal pain, and constipation; and low blood cell counts, which increase the risk of anemia, infection, bruising, or bleeding.
Stages
The stages of pancreatic cancer include:
Stage 0 (Carcinoma in Situ): Abnormal cells are found only in the lining of the pancreas.
Stage 1: Cancer is confined to the pancreas and can be surgically removed (resectable).
Stage 2: Cancer may have spread slightly beyond the pancreas—such as to nearby lymph nodes—and is resectable or borderline resectable.
Stage 3: Cancer is locally advanced, involving major arteries, making surgical removal more difficult.
Stage 4: Cancer is metastatic, having spread to distant organs such as the liver, and cannot be cured with surgery.
What Causes Pancreatic Cancer?
The pancreas is a 6-inch-long gland shaped like a thin, sideways pear. It has three parts: the head (wider end), body (middle), and tail (narrow end), and is located between the stomach and the spine.
Part of what makes pancreatic cancer so dangerous is the vital role the pancreas plays in the body. This organ is essential for digestion, producing enzymes that help break down food, and for regulating blood sugar levels through hormones such as insulin.
Pancreatic cancer can arise from different types of cells in the pancreas. Exocrine pancreatic cancers originate from cells that produce digestive enzymes and account for more than 95 percent of cases, with pancreatic ductal adenocarcinoma being the most common. Neuroendocrine tumors—also called islet cell tumors—develop from hormone-producing cells and make up less than 5 percent of cases.
While the exact cause of pancreatic cancer is unknown, many risk factors have been identified across several categories.
Genetic and Family History
Family history plays a significant role—up to 15 percent of cases are linked to it. Having a first-degree relative with pancreatic cancer increases risk by two to three times, and the likelihood multiplies with more affected family members. Those with a strong family history may be up to nine times more likely to develop pancreatic cancer.
Certain genetic conditions increase susceptibility, including familial atypical multiple mole melanoma syndrome; Peutz-Jeghers syndrome, which causes polyps in the stomach and intestines and distinctive dark spots on the face, lips, hands, and feet; Lynch syndrome (hereditary nonpolyposis colorectal cancer); and inherited mutations such as BRCA1, BRCA2, PALB2, and ATM. Hereditary pancreatitis, which causes repeated inflammation, significantly increases risk over time.
Lifestyle Risk Factors
These factors are largely controllable and represent the best opportunity for risk reduction:
Smoking: Linked to about 20 percent to 25 percent of pancreatic cancer cases. Smoking doubles the risk, and smoking-related tumors tend to grow faster and appear about 10 years earlier than those in nonsmokers. People who quit smoking 20 years ago have the same risk as those who never smoked.
Obesity: Having a body mass index (BMI) over 25 or 30, respectively, increases risk. Maintaining a healthy weight through diet and exercise helps protect against pancreatic cancer.
Heavy Alcohol Use: Drinking about three or more standard alcoholic beverages per day can lead to chronic pancreatitis and may increase cancer risk compared with lighter drinking.
High Sugar Intake: A 2019 study found that high-sugar environments increase the likelihood of gene mutations that lead to pancreatic cancer by five times compared with normal glucose levels.
Nighttime Artificial Light Exposure: A 2021 study showed that people in areas with the highest levels of artificial nighttime light had a 27 percent greater risk of pancreatic cancer compared to those in the least-lit regions.
Chemicals and Radiation: Chemical exposure to carcinogens such as asbestos, pesticides, dyes, and petrochemicals may increase risk. Ionizing radiation from high-energy sources such as X-rays or gamma rays is linked to a very small increased risk.
Medical Conditions
Several health conditions increase risk. While not entirely controllable, many can be managed with medical care:
Chronic Pancreatitis: Long-term pancreatic inflammation can affect people as young as 35 and may result from genetic factors, duct abnormalities, trauma, or long-term alcohol abuse.
Gallstones: Gallstones may increase risk by leading to chronic pancreatitis. Treating gallstone disease may help protect the pancreas.
Diabetes: Associated with a twofold increase in risk, though the connection isn’t fully understood. In some cases, diabetes may actually signal early pancreatic cancer rather than cause it. Proper diabetes management remains important regardless.
Insulin Resistance: Causes excess insulin production, which can overstimulate pancreatic cells and lead to inflammation, increasing the risk of those cells becoming precancerous.
Metabolic Syndrome: A cluster of conditions—including excess belly fat, high blood sugar (insulin resistance), high blood pressure, and elevated blood fat levels—that collectively raise cancer risk. This condition is often manageable through lifestyle changes.
Polycystic Ovary Syndrome (PCOS): A 2024 study found that PCOS was associated with a 38 percent increased risk of pancreatic cancer. Women with PCOS should discuss pancreatic screening options with their doctors.
Previous Cancers: May slightly increase risk, possibly due to past treatments, genetic factors, or lifestyle habits such as diet and smoking. Regular follow-up care is important for cancer survivors.
Certain Infections: Some infections—including hepatitis B, bacteria from gum disease, and Helicobacter pylori—may be linked to a higher risk, though evidence is still emerging. Treating these infections when possible is advisable.
COVID-19 Infection: A 2020 study found that the S2 subunit of the SARS-CoV-2 spike protein interacts with tumor suppressor genes such as BRCA1 and BRCA2, whose impaired function is linked to higher pancreatic cancer risk.