|
Getting your Trinity Audio player ready...
|
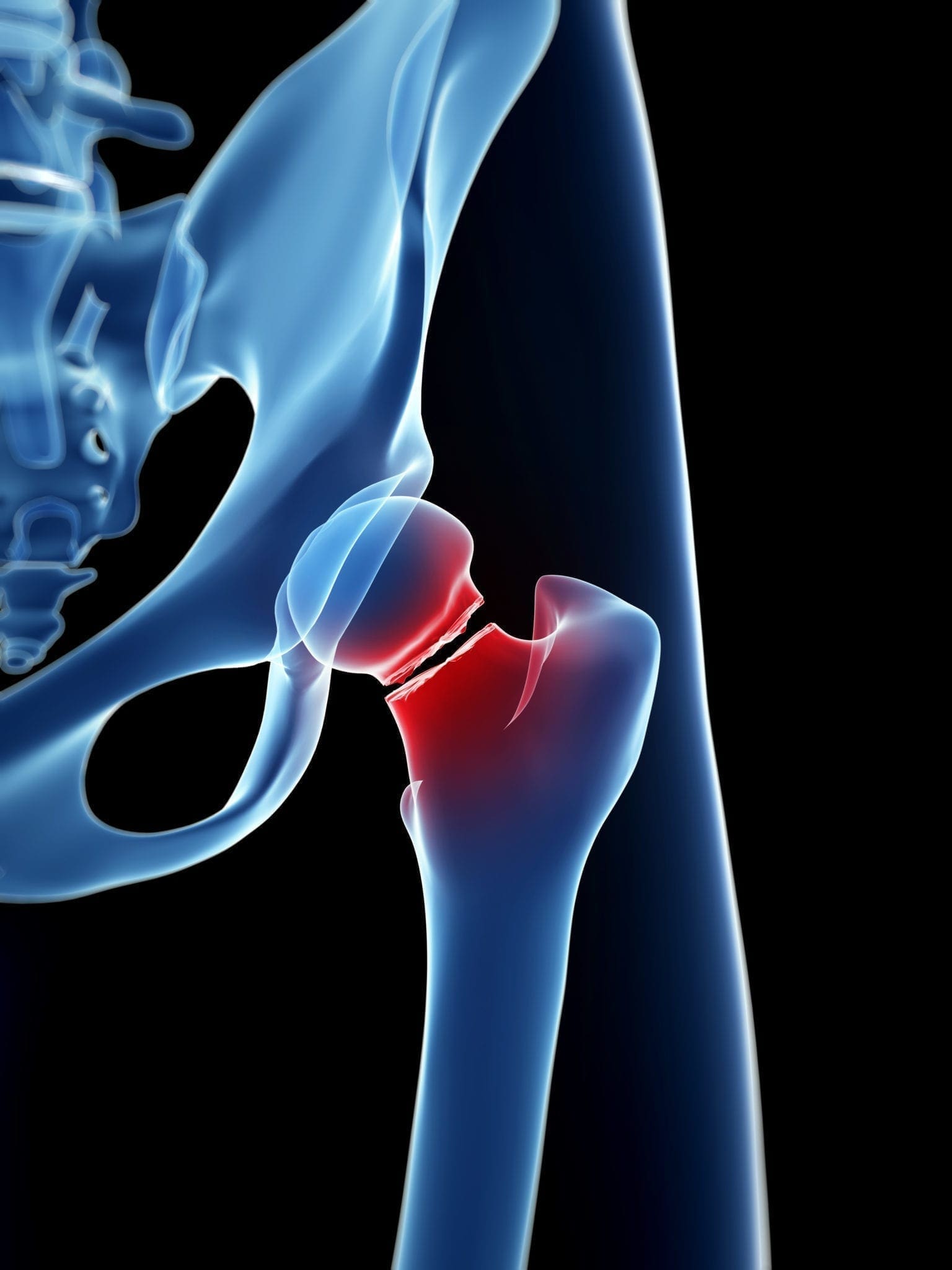
The potential for hip fractures increases as we age—taking preventative steps to reduce falling may reduce the risk.
By: Ellen Wan
In people over 50, the risk of osteoporosis-related fractures significantly increases, leading to a higher mortality rate. Recent studies have shown that the survival rate for elderly individuals after a hip fracture is even lower than that for colorectal cancer, the second leading cause of cancer death in the United States.
Hip fractures, often referred to as the “silent killer of the elderly,” occur when the femur (thigh bone) breaks near the hip joint. A recent study published in the Journal of Bone and Mineral Research Plus in May found that the survival rate for elderly individuals significantly decreases after a fracture, with hip fractures having the poorest prognosis.
Low Survival Rates of Hip Fractures
The study examined 98,474 patients aged 65 and older who experienced fractures at various sites between 2011 and 2015. These patients were matched 1:1 with a non-fracture cohort based on sex, age, rural or urban residence, and comorbidities associated with fracture risk. After up to six years of follow-up, researchers assessed the overall survival rate of the fracture patients and compared it to the relative survival rate of the non-fracture cohort.
The results showed that those with hip fractures had the lowest survival rates, followed by vertebral fractures. The one-year overall survival rate for hip fracture patients was 67.7 percent for men and 78.5 percent for women. For vertebral fracture patients, the one-year overall survival rate was 75.5 percent for men and 84.9 percent for women. In contrast, the one-year overall survival rate for participants without fractures remained above 90 percent for both sexes.
Among the hip fracture patients, less than one-third (32.3 percent) of men and less than half (44.7 percent) of women survived for more than five years. For vertebral fracture patients, the five-year overall survival rate was 37.6 percent for men and 54.1 percent for women.
Notably, patients aged 85 and older had the poorest prognosis. Specifically, men with hip fractures had the lowest five-year overall survival rate, at only 17.9 percent, while men with vertebral fractures had a survival rate of 19.7 percent. Women had slightly higher five-year overall survival rates, with 30 percent for hip fractures and 35.7 percent for vertebral fractures.
Additionally, the study found that compared to the non-fracture cohort, the five-year relative survival rate after a hip fracture was the lowest, at 49.9 percent for men and 65 percent for women. For vertebral fractures, the five-year relative survival rate was slightly higher, at 53.9 percent for men and 72.7 percent for women.
The study also showed that while the survival rate after a fracture was generally higher for women than for men, women were at a significantly higher risk of fractures and were also more likely to experience subsequent fractures. These subsequent fractures accounted for up to two-thirds of the total deaths among women with fractures.
Jacques Brown, the lead author of the study and a professor of medicine at Laval University in Canada, stated in a press release that “survival most dramatically declined within one month after most types of fracture, with a five-year survival being similar to or worse than some common cancers.”
In the study, researchers noted that in the regions where these participants lived, the five-year relative survival rates for cancer patients diagnosed between 2012 and 2016 were 94 percent for men with prostate cancer and 89 percent for women with breast cancer.
Among common types of cancer in the United States, the five-year relative survival rate for melanoma (skin cancer) is around 94 percent, while the five-year relative survival rate for colorectal cancer, the second leading cancer killer in the United States, is around 65 percent.
In comparison, the five-year relative survival rate for hip fractures in individuals aged 65 and older is lower than that of the cancers listed above.
Factors Contributing to Low Survival Rates in Fracture Patients
The study revealed that, in the year prior to their fractures, 32 to 45 percent of female patients and 7 to 14 percent of male patients had received treatment for osteoporosis, with a higher treatment rate among those with vertebral fractures. Furthermore, patients with vertebral fractures were the most likely to have a history of opioid treatment, which may be prescribed for pain related to osteoporosis, compared to those with fractures at other sites.
In addition to prior osteoporosis treatment, the researchers also discussed other reasons for the low survival rates among individuals aged 65 and older. For instance, subsequent fractures are a potential short-term factor in the reduced one-year survival rate, as an initial fracture increases the risk of further fractures. Perioperative complications in patients undergoing surgical treatment have also been shown to increase mortality in the first few months following a fracture. Furthermore, overall frailty in the elderly is linked to higher mortality rates, and this frailty may further progress after a fracture, creating a vicious cycle.

The researchers stated that the study focused on the prognosis of fracture patients and corresponding interventions to improve outcomes, thereby increasing survival rates among the elderly with fractures. Dr. Brown emphasized in the press release, “These observations highlight the urgency to change our attitude towards these patients and offer them secondary prevention interventions before hospital discharge, as recommended by the American Society for Bone and Mineral Research.”
Increased Risk of Hip Fractures with Age
According to Johns Hopkins Medicine, hip fractures are common in the United States, with 350,000 cases reported annually.
In younger individuals, hip fractures typically result from severe trauma such as car accidents. As people age, their bones become more fragile. After the age of 50, the incidence of hip fractures doubles every ten years. Therefore, most hip fractures occur in those over 60, with falls being the most common cause among the elderly.
5 Preventive Steps to Reduce the Risk of Hip Fractures
Hip fractures in the elderly can cause various complications, increasing the risk of death. They also make recovery more difficult, potentially leading to a loss of independence, a decline in quality of life, and depression.
Dr. Deborah Sellmeyer, the medical director of the Johns Hopkins Metabolic Bone Center, stated on the official website, “Older adults can have life-threatening complications during or after surgery to treat a hip fracture, such as blood clots, infections and heart arrhythmias.” She emphasized the importance of taking all possible measures to prevent fractures, particularly hip fractures. Here are five steps you can take to effectively reduce your risk of hip fractures:
- Screen for bone density and maintain bone strength: It is recommended that all women aged 65 and older, as well as younger women at higher risk for fractures, undergo bone density testing. Dr. Sellmeyer noted that screening for osteoporosis allows your doctor to develop a treatment plan to keep your bones strong and prevent fractures.
Men over the age of 70, or those who have been using corticosteroid medications like prednisone for an extended period, are at increased risk of bone thinning and should talk to their doctors about osteoporosis screening.
- Keep muscles strong: Engaging in exercises that build muscle strength, endurance, and balance can help reduce the risk of fractures caused by slipping, tripping, or falling. One study found that regular exercise can lower the risk of falls in the elderly by 14.3 percent.
- Ensure adequate nutrition for bone health: Women under 50 and men under 70 should aim for 1,000 milligrams (mg) of calcium daily, while women over 50 and men over 70 should aim for 1,200 mg per day. Dr. Sellmeyer pointed out that vitamin D is essential for calcium absorption. It is recommended to take 600 IU of vitamin D daily before age 70 and 800 IU daily after age 70. This combination can significantly reduce the risk of fractures.
Additionally, it is important to eat plenty of potassium-rich fruits and vegetables, such as bananas and spinach. An earlier study by Dr. Sellmeyer and her colleagues found that potassium has a positive effect on calcium metabolism. Furthermore, protein also helps maintain muscle mass and supports bone growth.
- Check medications and vision: If you experience dizziness, lightheadedness, weakness, or loss of balance while walking, consult your doctor to review your medications, as some prescriptions may have side effects that increase the risk of falls. Additionally, make sure to have regular eye exams and update your glasses prescription as needed, as clear vision can help prevent falls.
- Improve home safety: Most falls occur at home, and simple changes can significantly reduce the risk. For example, keep floors and stairs free of clutter and consider installing handrails on stairs. Use non-slip mats in bathtubs and on bathroom floors, and install grab bars in the bathtub and shower. Remove throw rugs and enhance lighting. Additionally, walking barefoot or in socks can increase the risk of falls, so it is suggested to wear well-fitting shoes at home.





